Diabetes is a very serious ailment and there is an awful lot important information that you need to know, so we will provide the information to you in TWO different posts. For more information please visit the Mayo Clinic website where some of this information was taken from.
Diabetes is a very serious ailment and there is an awful lot important information that you need to know, so we will provide the information to you in TWO different posts. For more information please visit the Mayo Clinic website where some of this information was taken from.
The World Health Organization says that 90 percent of the estimated 171 million diabetics in the world are type 2 diabetics. A diabetic dies every 10 seconds, according to WHO.
Post 1 of 2
How Big Of A Problem Is it?
The World Health Organization says that 90 percent of the estimated 171 million diabetics in the world are type 2 diabetics. A diabetic dies every 10 seconds, according to WHO.
Definition: What is Diabetes?
The term “diabetes mellitus” refers to a group of diseases that affect how your body uses blood glucose, commonly called blood sugar. Glucose is vital to your health because it’s the main source of energy for the cells that make up your muscles and tissues. It’s your body’s main source of fuel.
If you have diabetes, no matter what type, it means you have too much glucose in your blood, although the reasons may differ. Too much glucose can lead to serious health problems.
Chronic diabetes conditions include type 1 diabetes and type 2 diabetes. Potentially reversible diabetes conditions include prediabetes — when your blood sugar levels are higher than normal, but not high enough to be classified as diabetes — and gestational diabetes, which occurs during pregnancy.
Symptoms: What you should be looking for!
Diabetes symptoms vary somewhat, depending on what type of diabetes you have. If you have prediabetes or gestational diabetes, you may not experience symptoms. Or you might experience some or all of the symptoms of type 1 and type 2 diabetes:
* Blurry vision
* Excessive thirst
* Fatigue
* Frequent urination
* Extreme Hunger
* Fatigue
* Nausea
* Vomiting
* Weight loss in spite of increased appetite
* Slow-healing sores
* Frequent infections, such as gum or skin infections and vaginal or bladder infections
Although type 1 diabetes can develop at any age, it typically appears during childhood or adolescence. Type 2 diabetes, the most common type, can develop at any age and is often preventable.
When to see a doctor
* If you suspect you may have diabetes. If you notice any possible diabetes symptoms, contact your doctor. The earlier the condition is diagnosed, the sooner treatment can begin.
* If you’ve already been diagnosed with diabetes. If you’ve been diagnosed with diabetes, you’ll need close medical follow-up until your blood sugar levels stabilize.
What Causes Diabetes?
To understand diabetes, first you must understand how glucose is normally processed in the body.
 How glucose normally works
How glucose normally works
Glucose is a main source of energy for the cells that make up your muscles and other tissues. Glucose comes from two major sources: the food you eat and your liver. During digestion, sugar is absorbed into the bloodstream. Normally, sugar then enters cells with the help of insulin.
The hormone insulin comes from the pancreas, a gland located just behind the stomach. When you eat, your pancreas secretes insulin into your bloodstream. As insulin circulates, it acts like a key by unlocking microscopic doors that allow sugar to enter your cells. Insulin lowers the amount of sugar in your bloodstream. As your blood sugar level drops, so does the secretion of insulin from your pancreas.
Your liver acts as a glucose storage and manufacturing center. When you haven’t eaten in a while, for example, your liver releases stored glucose to keep your glucose level within a normal range.
Causes of type 1 diabetes
In type 1 diabetes, your immune system — which normally fights harmful bacteria or viruses — attacks and destroys the insulin-producing cells in the pancreas. This leaves you with little or no insulin. Instead of being transported into your cells, sugar builds up in your bloodstream.
Causes of prediabetes and type 2 diabetes
In prediabetes — which can lead to type 2 diabetes — and in type 2 diabetes, your cells become resistant to the action of insulin, and your pancreas is unable to make enough insulin to overcome this resistance. Instead of moving into your cells, sugar builds up in your bloodstream. Exactly why this happens is uncertain, although excess fat — especially abdominal fat — and inactivity seem to be important factors.
Causes of gestational diabetes
During pregnancy, the placenta produces hormones to sustain your pregnancy. These hormones make your cells more resistant to insulin. As your placenta grows larger in the second and third trimesters, it secretes more of these hormones — making it even harder for insulin to do its job.
Normally, your pancreas responds by producing enough extra insulin to overcome this resistance. But sometimes your pancreas can’t keep up. When this happens, too little glucose gets into your cells and too much stays in your blood. This is gestational diabetes.
Risk factors
Risk factors for diabetes depend on the type of diabetes.
Risk factors for type 1 diabetes
Although the exact cause of type 1 diabetes is unknown, family history may play a role. Your risk of developing type 1 diabetes increases if you have a parent or sibling who has type 1 diabetes. Other factors have been proposed, as well, such as exposure to a viral illness.
Risk factors for prediabetes and type 2 diabetes
Researchers don’t fully understand why some people develop prediabetes and type 2 diabetes and others don’t. It’s clear that certain factors increase the risk, however, including:
* Weight. The more fatty tissue you have, the more resistant your cells become to insulin.
* Inactivity. The less active you are, the greater your risk. Physical activity helps you control your weight, uses up glucose as energy and makes your cells more sensitive to insulin.
* Family history. Your risk increases if a parent or sibling has type 2 diabetes.
* Race. Although it’s unclear why, people of certain races — including blacks, Hispanics, American Indians and Asian-Americans — are at higher risk.
* Age. Your risk increases as you get older, especially after age 45. Often, that’s because you tend to exercise less, lose muscle mass and gain weight as you age. But type 2 diabetes is increasing dramatically among children, adolescents and younger adults.
* Gestational diabetes. If you developed gestational diabetes when you were pregnant, your risk of developing prediabetes and type 2 diabetes later increases. If you gave birth to a baby weighing more than 9 pounds (4 kilograms), you’re also at risk of type 2 diabetes.
* Polycystic ovary syndrome. For women, having polycystic ovary syndrome — a common condition characterized by irregular menstrual periods, excess hair growth and obesity — increases the risk of diabetes.
Other conditions associated with diabetes include:
* High blood pressure
* High levels of low-density lipoprotein (LDL), or “bad,” cholesterol
* Low levels of high-density lipoprotein (HDL), or “good,” cholesterol
* High levels of triglycerides, another fat in the blood
When these conditions — high blood pressure, high blood sugar and abnormal blood fats — occur together with obesity, they are associated with resistance to insulin.
Risk factors for gestational diabetes
Any pregnant woman can develop gestational diabetes, but some women are at greater risk than are others. Risk factors for gestational diabetes include:
* Age. Women older than age 25 are at increased risk.
* Family or personal history. Your risk increases if you have prediabetes — a precursor to type 2 diabetes — or if a close family member, such as a parent or sibling, has type 2 diabetes. You’re also at greater risk if you had gestational diabetes during a previous pregnancy, if you delivered a very large baby or if you had an unexplained stillbirth.
* Weight. Being overweight before pregnancy increases your risk.
* Race. For reasons that aren’t clear, women who are black, Hispanic, American Indian or Asian are more likely to develop gestational diabetes.
Complications, How Bad Can It Get?
Diabetes complications vary depending on the type of diabetes you have.
Complications of type 1 and type 2 diabetes
 Short-term complications of type 1 and type 2 diabetes require immediate care. Left untreated, these conditions can cause seizures and a state of unconsciousness (coma).
Short-term complications of type 1 and type 2 diabetes require immediate care. Left untreated, these conditions can cause seizures and a state of unconsciousness (coma).
* High blood sugar (hyperglycemia). Your blood sugar level can rise for many reasons, including eating too much, being sick or not taking enough glucose-lowering medication.
* Increased ketones in your urine (diabetic ketoacidosis). If your cells are starved for energy, your body may begin to break down fat. This produces potentially toxic acids known as ketones.
* Low blood sugar (hypoglycemia). If your blood sugar level drops below your target range, it’s known as low blood sugar. Your blood sugar level can drop for many reasons, including skipping a meal and getting more physical activity than normal. However, low blood sugar is most likely if you take glucose-lowering medications that promote the secretion of insulin or if you’re receiving insulin therapy.
Long-term complications of diabetes develop gradually. The earlier you develop diabetes — and the less controlled your blood sugar — the higher the risk of complications. Eventually, diabetes complications may be disabling or even life-threatening.
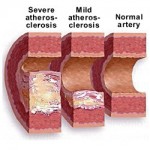
* Cardiovascular disease. Diabetes dramatically increases the risk of various cardiovascular problems, including coronary artery disease with chest pain (angina), heart attack, stroke and narrowing of arteries (atherosclerosis). If you have diabetes, you are twice as likely to have heart disease or stroke.
* Nerve damage (neuropathy). Excess sugar can injure the walls of the tiny blood vessels (capillaries) that nourish your nerves, especially in the legs. This can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and over a period of months or years gradually spreads upward. Left untreated, you could lose all sense of feeling in the affected limbs. Damage to the nerves related to digestion can cause problems with nausea, vomiting, diarrhea or constipation. For men, it may lead to problems with erectile dysfunction.
* Kidney damage (nephropathy). The kidneys contain millions of tiny blood vessel clusters (glomeruli) that filter waste from your blood. Diabetes can damage this delicate filtering system. Severe damage can lead to kidney failure or irreversible end-stage kidney disease, requiring dialysis or a kidney transplant.
* Eye damage. Diabetes can damage the blood vessels of the retina (diabetic retinopathy), potentially leading to blindness.
* Foot damage. Nerve damage in the feet or poor blood flow to the feet increases the risk of various foot complications. Left untreated, cuts and blisters can become serious infections. Severe damage might require toe, foot or even leg amputation.
* Skin and mouth conditions. Diabetes may leave you more susceptible to skin problems, including bacterial infections, fungal infections and itching. Gum infections also may be a concern, especially if you have a history of poor dental hygiene.
* Bone and joint problems. Diabetes may put you at risk of bone and joint problems such as osteoporosis.
Complications of gestational diabetes
Most women who have gestational diabetes deliver healthy babies. However, untreated or uncontrolled blood sugar levels can cause problems for you and your baby.
Complications in your baby can occur as a result of gestational diabetes:
* Excess growth. Extra glucose can cross the placenta, which triggers your baby’s pancreas to make extra insulin. This can cause your baby to grow too large (macrosomia). Very large babies are more likely to become wedged in the birth canal, sustain birth injuries or require a C-section birth.
* Low blood sugar. Sometimes babies of mothers with gestational diabetes develop low blood sugar (hypoglycemia) shortly after birth because their own insulin production is high. Prompt feedings and sometimes an intravenous glucose solution can return the baby’s blood sugar level to normal.
* Respiratory distress syndrome. If your baby is delivered early, respiratory distress syndrome — a condition that makes breathing difficult — is possible. Babies who have respiratory distress syndrome may need help breathing until their lungs become stronger.
* Jaundice. This yellowish discoloration of the skin and the whites of the eyes may occur if a baby’s liver isn’t mature enough to break down a substance called bilirubin, which normally forms when the body recycles old or damaged red blood cells. Although jaundice usually isn’t a cause for concern, careful monitoring is important.
* Type 2 diabetes later in life. Babies of mothers who have gestational diabetes have a higher risk of developing obesity and type 2 diabetes later in life.
* Death. Rarely, untreated gestational diabetes results in a baby’s death either before or shortly after birth.
Complications in you can also occur as a result of gestational diabetes:
* Preeclampsia. This condition is characterized by high blood pressure and excess protein in the urine. Left untreated, preeclampsia can lead to serious or even life-threatening complications for both mother and baby.
* Subsequent gestational diabetes. Once you’ve had gestational diabetes in one pregnancy, you’re more likely to have it again with the next pregnancy. You’re also more likely to develop diabetes — typically type 2 diabetes — as you get older.
Complications of prediabetes
Prediabetes may develop into type 2 diabetes.
Tests and diagnosis
Tests for type 1 and type 2 diabetes
In June 2009, an international committee composed of experts from the American Diabetes Association, the European Association for the Study of Diabetes and the International Diabetes Federation recommended that type 1 and type 2 diabetes testing include the:
* Glycated hemoglobin (A1C) test. This blood test indicates your average blood sugar level for the past two to three months. It works by measuring the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells. The higher your blood sugar levels, the more hemoglobin you’ll have with sugar attached. An A1C level of 6.5 percent or higher on two separate tests indicates you have diabetes.
If the A1C test isn’t available, or if you have certain conditions that can make the A1C test inaccurate — such as if you’re pregnant or have an uncommon form of hemoglobin (known as a hemoglobin variant) — your doctor may use the following tests to diagnose diabetes:
* Random blood sugar test. A blood sample will be taken at a random time. Regardless of when you last ate, a random blood sugar level of 200 milligrams per deciliter (mg/dL) — 11.1 millimoles per liter (mmol/L) — or higher suggests diabetes.
* Fasting blood sugar test. A blood sample will be taken after an overnight fast. A fasting blood sugar level between 70 and 99 mg/dL (3.9 and 5.5 mmol/L) is normal. If it’s 126 mg/dL (7 mmol/L) or higher on two separate tests, you’ll be diagnosed with diabetes.
Tests for gestational diabetes
Screening for gestational diabetes is a routine part of prenatal care. Most health care providers recommend a blood test known as a glucose challenge test between the 24th and 28th weeks of pregnancy — or earlier if you’re at particularly high risk of gestational diabetes.
You’ll begin the glucose challenge test by drinking a syrupy glucose solution. One hour later, you’ll have a blood test to measure your blood sugar level. A blood sugar level above 140 mg/dL (7.8 mmol/L) usually indicates gestational diabetes, but you’ll likely need a second test to confirm the diagnosis.
For the follow-up test, you’ll be asked to fast overnight. Then you’ll drink another sweet solution — this one containing a higher concentration of glucose — and your blood sugar level will be checked every hour for a period of three hours.
Tests for prediabetes
The American College of Endocrinology suggests prediabetes testing for anyone who has a family history of type 2 diabetes and for those who are obese or have metabolic syndrome. Women with a personal history of gestational diabetes also should be tested.
The primary test to screen for prediabetes is the:
* Glycated hemoglobin (A1C) test. This blood test indicates your average blood sugar level for the past two to three months. It works by measuring the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells. The higher your blood sugar levels, the more hemoglobin you’ll have with sugar attached. An A1C level between 6 and 6.5 percent suggests you have prediabetes.
If the A1C test isn’t available, or if you have certain conditions that can make the A1C test inaccurate — such as if you’re pregnant or have an uncommon form of hemoglobin (known as a hemoglobin variant) — your doctor may use the following tests to diagnose diabetes:
* Fasting blood sugar test. A blood sample will be taken after an overnight fast. A blood sugar level from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes.
* Oral glucose tolerance test. A blood sample will be taken after you fast for at least eight hours or overnight. Then you’ll drink a sugary solution, and your blood sugar level will be measured again after two hours. A blood sugar level less than 140 mg/dL (7.8 mmol/L) is normal. A blood sugar level from 140 to 199 mg/dL (7.8 to 11 mmol/L) is considered prediabetes. This is sometimes referred to as impaired glucose tolerance (IGT). A blood sugar level of 200 mg/dL (11.1 mmol/L) or higher may indicate diabetes.
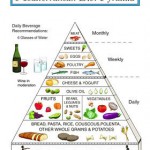
Please read post 2of2 where we discuss how to naturally fight Diabetes!